by Ariayana Harrell, Intern and UNC Psychology Major
If you have not watched our podcast about trauma that was released earlier this week, I would highly recommend watching it before reading this post! This post will discuss some of the major kinds of therapies that are used for treating trauma. This is not an exhaustive list, but these are some of the more popular therapies!
Narrative Therapies
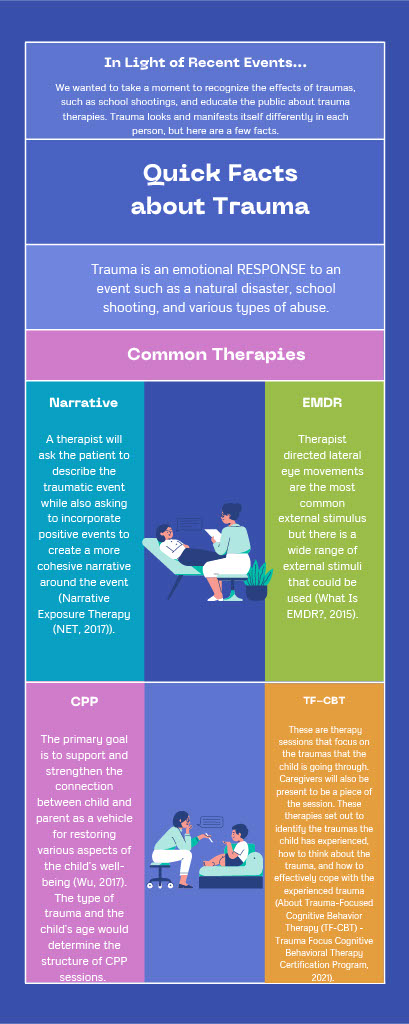
Narrative exposure therapies are commonly used for treating trauma disorders such as PTSD (Narrative Exposure Therapy (NET, 2017)). This type of therapy is often completed in groups; however, it is not uncommon for someone to undergo this kind of treatment without a group (individually). How does this work? A therapist will ask the patient to describe the traumatic event while also asking to incorporate positive events to create a more cohesive narrative around the event.
This is so the patient can recognize that there is more context to the traumatic event, so they will be able to give less power to the traumatic event and start seeing a “bigger picture.” Hopefully, by discussing the traumatic event, the patient will be more comfortable discussing the event and discussing how they felt because of the event. From here, treatment will be more centered around the event and the patient (Narrative Exposure Therapy (NET, 2017)).
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is an eight-phase treatment and is primarily used on adults because of the methods that are used in this treatment. A client would “tap into” their emotionally disturbing event while also focusing on an external stimulus such as following the therapist’s finger from side to side. Therapist directed lateral eye movements are the most common external stimulus but there is a wide range of external stimuli that could be used (What Is EMDR? – EMDR Institute – EYE MOVEMENT DESENSITIZATION and REPROCESSING THERAPY, 2015).
- Phase 1: history taking sessions.
- Phase 2: Therapist educates the client about the various ways of dealing with emotional distress.
- Phases 3-6: Target is identified and processed using the vivid visual image related to the memory, negative beliefs about self, and related emotions and body sensations.
- Phase 7: Closure
- Phase 8: Examining the process made
Eye movements are used during one part of the session, and after the clinician determines which memory to focus on first, then they will ask the client to hold different thoughts or aspects of that event and use their eyes to track the therapist’s hands. Some scientists believe that biological mechanisms in rapid eye movement (REM) sleep are connected to the effectiveness of the client being able to recall the traumatic event while also following the clinician’s hand movement.
A successful EMDR therapy would transform the meaning of painful events on an emotional level. For example, a person who was abused mentally, sexually, physically, and/or verbally would no longer feel disgusted with themselves, but rather, they would be able to walk out of the treatment being able to say, “I am strong. I can fight this. I have survived.” (What Is EMDR? – EMDR Institute – EYE MOVEMENT DESENSITIZATION and REPROCESSING THERAPY, 2015).
Trauma-Focused Cognitive Behavior Therapy (TF-CBT)
TFCBT is a short-term treatment model that helps children and adolescents recover after trauma. Usually, treatment lasts for 8-25 sessions with the child/adolescent and caregiver (About Trauma-Focused Cognitive Behavior Therapy (TF-CBT) – Trauma Focus Cognitive Behavioral Therapy Certification Program, 2021). This is exactly what it sounds like! These are therapy sessions that focus on the traumas that the child is going through. Caregivers will also be present to be a piece of the session.
These therapies set out to identify the traumas the child has experienced, how to think about the trauma, and how to effectively cope with the experienced trauma. Additionally, it helps the family better understand how to care for their child and how to provide the proper resources for their child. For more information, here is a peer-reviewed article that goes into more detail about TF-CBT: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4476061/!
Child-Parent Psychotherapy (CPP)
CPP is therapy primarily used for children from birth through age five who have experienced trauma and their caregivers. This is very similar to TF-CBT; however, CPP is based on attachment theory but also integrates psychodynamic, developmental, trauma, social learning, and cognitive behavior theories. The primary goal is to support and strengthen the connection between child and parent as a vehicle for restoring various aspects of the child’s well-being (Wu, 2017).
The type of trauma and the child’s age would determine the structure of CPP sessions. These sessions are conducted by a therapist who is certified. These sessions are typically hour-long weekly sessions, but the length of treatment varies between clients.
In conclusion, there are many different types of therapies to help treat and cope with emotional distress and trauma. Some therapies work better for children, but that does not mean those treatments would not work for people of other ages. One should look for a therapist who are trained and certified in these areas if they are planning or actively seeking treatment for trauma.
Each method has its pros and cons, so when choosing which treatment, be sure to fully weigh your options and do not be afraid to switch treatments if you feel the one you have chosen is not working for you. However, make sure you are giving adequate time for the treatment to work. Nothing will be solved immediately. Be patient!
References
About Trauma-Focused Cognitive Behavior Therapy (TF-CBT) – Trauma Focus Cognitive Behavioral Therapy Certification Program. (2021, March 26). Trauma Focus Cognitive Behavioral Therapy Certification Program. https://tfcbt.org/about/.
Narrative Exposure Therapy (NET. (2017). Narrative Exposure Therapy (NET). Https://Www.apa.org. https://www.apa.org/ptsd-guideline/treatments/narrative-exposure-therapy.
What is EMDR? – EMDR Institute – EYE MOVEMENT DESENSITIZATION AND REPROCESSING THERAPY. (2015, February 15). EMDR Institute – EYE MOVEMENT DESENSITIZATION and REPROCESSING THERAPY. https://www.emdr.com/what-is-emdr/.
Wu, J. (2017, August 28). Child-Parent Psychotherapy. The National Child Traumatic Stress Network. https://www.nctsn.org/interventions/child-parent-psychotherapy.
Written by:
Ariayana Harrell, UNC Class of 2023
Psychology B.S and Sociology B.A
Women and Gender Studies Minor